Male fertility plays a crucial role in reproductive success, yet many men remain unaware of the factors influencing their sperm health and count. This blog unpacks the essentials of male fertility, from how sperm is produced to common causes behind low sperm count. We explore how lifestyle choices, medical issues, environmental exposures, and nutrition all intersect to impact reproductive outcomes. Psychological stress and new advances in diagnosis and treatment also shape this complex picture. Together, these interconnected aspects offer a comprehensive understanding of what affects male fertility and how it can be supported or improved.
Understanding the Basics of Male Fertility and Sperm Production
Understanding the basics of male fertility and sperm production is essential to grasp how various factors influence reproductive potential. This foundational knowledge covers the complex process of sperm development in the testes, including hormone regulation and the critical stages of maturation that determine sperm quality and count. A clear understanding here sets the stage for exploring common causes of low sperm count, such as hormonal imbalances or genetic issues discussed later. It also highlights why lifestyle choices and environmental exposures profoundly affect sperm health by disrupting these biological processes. Moreover, recognizing how medical conditions or treatments interfere with sperm production connects directly to sections on health impacts and emerging therapies. Nutritional support and stress management further tie back to this foundation by influencing hormonal balance and cellular function essential for healthy sperm formation. By starting with these basics, readers can better appreciate the intricate interplay of factors shaping male fertility outcomes throughout the blog.
Common Causes of Low Sperm Count and Impaired Fertility

Common causes of low sperm count and impaired fertility encompass a variety of factors that directly disrupt sperm production, quality, and function. These causes often stem from underlying medical conditions such as hormonal imbalances or varicocele, which are explored in detail under medical conditions and treatments impacting male fertility. Lifestyle habits including smoking, excessive alcohol consumption, and poor diet also play a critical role, linking closely to the lifestyle influences and nutritional factors sections. Environmental exposures to toxins and heat further contribute to diminished sperm health, highlighting the importance of understanding external risks covered elsewhere in the blog. Psychological stress can alter hormone levels and reduce reproductive potential, connecting with the section on mental well-being’s impact on fertility. By examining these intertwined causes within a holistic framework—including advancements in diagnosis and therapies—the blog offers a comprehensive view of what compromises male reproductive capacity and how it might be addressed effectively.
Lifestyle Influences on Sperm Quality and Reproductive Success
Lifestyle choices profoundly influence sperm quality and overall reproductive success, making this aspect a critical focus within male fertility discussions. Habits such as smoking, excessive alcohol intake, poor diet, and lack of exercise can significantly reduce sperm count and motility, directly connecting to the nutritional factors explored in the blog. Additionally, prolonged exposure to heat from tight clothing or frequent hot baths may impair sperm production, intersecting with environmental influences detailed elsewhere. Psychological stress also plays a pivotal role by disrupting hormone balance and sperm function, linking closely to the section on mental health impacts. Recognizing these lifestyle elements helps contextualize medical causes and treatments affecting fertility while emphasizing prevention through healthier living. By integrating lifestyle modifications alongside emerging diagnostic tools and therapies discussed later in the blog, men can achieve improved reproductive outcomes and better understand how everyday decisions shape their fertility potential.
Medical Conditions and Treatments Impacting Male Fertility

Medical conditions and their treatments play a significant role in shaping male fertility by directly influencing sperm production, quality, and function. Disorders such as varicocele, hormonal imbalances, infections, and genetic abnormalities can impair sperm health, often leading to reduced sperm count or motility. Additionally, therapies like chemotherapy or radiation for cancer may cause temporary or permanent damage to the testes, further complicating reproductive potential. Understanding these medical factors complements insights from lifestyle influences and environmental exposures that also impact sperm vitality. For men facing such challenges, advancements in diagnosis and emerging therapies offer promising options to restore or enhance fertility. Integrating knowledge of nutritional support and stress management can bolster treatment outcomes by improving overall reproductive health. This comprehensive view highlights how addressing medical conditions is crucial within the broader context of factors affecting male fertility discussed throughout the blog.
The Role of Environmental Exposures in Shaping Sperm Health and Fertility Outcomes
Environmental exposures play a significant role in shaping sperm health and overall fertility outcomes, often interacting with lifestyle choices and underlying medical conditions to influence reproductive success. Toxins such as pesticides, heavy metals, and air pollutants can disrupt sperm production by causing oxidative stress or hormonal imbalances, factors also discussed in the context of common causes of low sperm count. These external influences may compound issues stemming from poor nutrition or psychological stress, further impairing sperm quality. Understanding how these environmental risks intersect with other determinants of male fertility—such as those outlined in sections on lifestyle influences and medical treatments—provides a comprehensive picture of factors that affect sperm function. This insight is crucial for developing targeted interventions and aligns closely with advancements in diagnosis and emerging therapies aimed at mitigating the impact of harmful exposures to improve reproductive outcomes.
Nutritional Factors and Supplements That Support Optimal Sperm Function

Nutritional factors and targeted supplements play a crucial role in supporting optimal sperm function, complementing insights from lifestyle and medical influences discussed earlier in the blog. Essential nutrients such as zinc, selenium, folate, and antioxidants like vitamins C and E help protect sperm from oxidative damage while promoting healthy development and motility. Omega-3 fatty acids also contribute to membrane fluidity, which is vital for sperm vitality. These nutritional elements can mitigate some effects outlined in sections covering environmental exposures or psychological stress by enhancing cellular resilience. Moreover, understanding how diet intersects with common fertility challenges deepens the foundation laid out in discussions about low sperm count causes. While medical treatments address underlying conditions, proper supplementation offers a proactive approach to improve sperm quality naturally. Integrating nutritional strategies thus forms an integral part of a holistic framework for male reproductive health alongside emerging therapies highlighted later in the blog.
Psychological Stress and Its Effects on Male Reproductive Health
Psychological stress plays a significant role in male reproductive health by disrupting hormonal balance and impairing sperm production. Chronic stress elevates cortisol levels, which can interfere with the secretion of testosterone and other hormones critical for spermatogenesis, linking closely to the foundational concepts discussed in “Understanding the Basics of Male Fertility and Sperm Production.” Stress may also contribute to lifestyle factors such as poor sleep, unhealthy diet, or reduced physical activity, echoing themes from “Lifestyle Influences on Sperm Quality and Reproductive Success.” Additionally, prolonged psychological strain can exacerbate medical conditions outlined in “Medical Conditions and Treatments Impacting Male Fertility,” further compromising fertility outcomes. By influencing both physiological and behavioral pathways, stress underscores the complex interplay between mental well-being and reproductive function. Recognizing this connection complements insights from sections on nutrition, environmental exposures, and emerging therapies, highlighting the need for holistic approaches that address both mind and body to optimize sperm health.
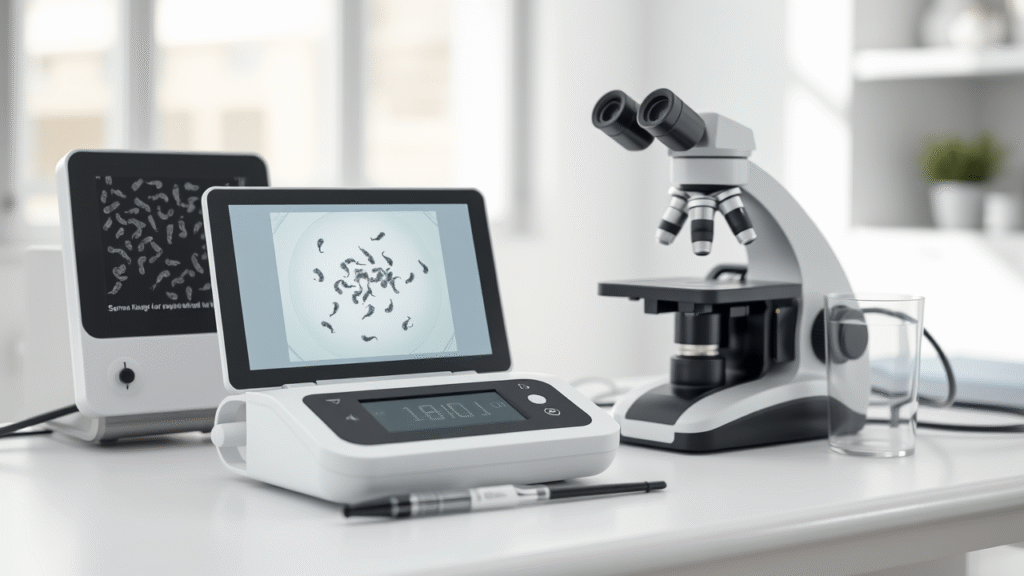
Advancements in Diagnosis and Emerging Therapies for Enhancing Male Fertility
As diagnostic tools become more precise and therapies evolve, the landscape of male fertility care is shifting toward personalized, effective solutions. These advancements not only address underlying medical causes but also complement lifestyle and environmental considerations explored earlier. Together, they offer renewed hope for those navigating fertility challenges, emphasizing that sperm health is influenced by a complex interplay of factors. Through understanding and innovation, men can find clearer paths to reproductive well-being. At MomDadDispatch.com, we recognize these journeys with empathy and support every step of the way.